What is ERCP and Surgical Endoscopy?
ERCP (Endoscopic Retrograde Cholangiopancreatography) and surgical endoscopy are special endoscopic procedures used to diagnose and treat digestive system diseases. Since it offers a minimally invasive approach in diagnosis and treatment, especially in the treatment of post-surgical complications, it increases the chance of both correct diagnosis and definitive treatment in early tumors, and contributes to the treatment of complications that develop after major surgeries, greatly reducing surgery-related mortality rates.
ERCP is an advanced endoscopy procedure that generally provides access to the liver, bile ducts and pancreas and is indispensable for HPB Surgery. It is used in the diagnosis and treatment of diseases such as bile duct stones, acute and chronic pancreatitis, bile duct obstructions, bile leaks that develop after surgery-related bile duct injuries, bile duct and pancreatic cancer. ERCP is usually performed by entering through the mouth with a flexible endoscope. There is a camera at the end of the endoscope that allows surgeons to see the internal organs and channels where the procedure can be performed.
Advanced ERCP is mostly used in the treatment of severe pancreatitis complications such as Pseudocysts and walled pancreatic necrosis (Pancreatic WON), non-surgical removal of benign or early stage tumors of the papilla such as endoscopic ampullectomy, ERCP procedures in patients who have undergone stomach surgery such as Billrot II, and treatment of biliary and pancreatic complications after major HPB surgery.
Surgical Endoscopy is a minimally invasive endoscopic procedure performed with special gastroscopes and colonoscopes. It provides the opportunity to view and intervene in the entire gastrointestinal system. It also enables surgical intervention with endoscopic tools without making large incisions in the organs. ERCP and Advanced Surgical Endoscopy applications are performed by General Surgeons, Internists, Radiologists and Gastroenterologists who have received training in this field, called Gastrointestinal Endoscopists in developed countries.
ERCP
Endoscopic retrograde cholangiopancreatography (ERCP) is based on the principle of entering the mouth with a special endoscope and imaging the bile ducts and pancreatic ducts under x-ray with special catheters inside this endoscope. McCune, an American surgeon, first reported endoscopic imaging (ERCP) of the choledoch and pancreatic duct in 1968. He stated that the characteristics that doctors who would perform this procedure should have were Honesty, Impartiality and Inexhaustible Patience. 5 years later, German and Japanese gastroenterologists defined endoscopic sphincterotomy and stone extraction. Since then, with the contribution of the great advancement of technology, ERCP has become an indispensable method in the diagnosis as well as the treatment of bile duct and pancreatic duct diseases. Today, despite methods such as endoscopic sonography (EUS), CT, MRI-MRCP and PTK, the importance of ERCP has not decreased, but it is used more for therapeutic, i.e. treatment purposes.
ERCP is most commonly performed for the non-surgical removal of gallstones that have fallen into the bile ducts (choledocholithiasis), but it is also a method used in the treatment of cholangitis, biliary tract inflammation, pancreatitis and obstructive jaundice due to pancreatic and biliary tract tumors. In addition, it is a life-saving method in the treatment of bile and pancreatic fluid leaks that may occur after liver, bile and pancreas surgeries or jaundice due to bile duct injuries, and in the non-surgical treatment of pseudocysts and walled necrosis (WON), which are fluid accumulations in the abdomen in severe pancreatic inflammation.
ERCP intervention is performed using a videoendoscopic device, a side-view Duodenoscope, and a C-arm X-ray or angiography device. The procedure is performed in 10-30 minutes with the assistance of an anesthesiologist. The patient is placed on the X-ray table in the left lateral position and entered through the mouth. The esophagus and stomach are passed and the duodenoscope is fixed in the second part of the duodenum, where the bile ducts open into the intestines, called the papilla major. The bile duct and pancreatic duct are visualized using a cannula, sphincterotome, guidewire, balloon and a special catheter called a basket: If there is a stone, it is dropped into the intestine or if the stone is large, it is broken with a lithotripter; if there is a tumor, stenosis or biliary fistula, a stent is placed with ERCP, and if necessary, the stenosis is widened with a balloon.
Before the procedure, the patient is examined and the necessary tests are seen. The person who will undergo ERCP must be fasting for at least 8 hours before the procedure. In addition, if there are blood thinning medications such as Plavix, Aspirin, Coumadin, these should be stopped 5-7 days before the procedure.
Procedures performed during ERCP:
- Endoscopic cholangiopancreatography
- Endoscopic sphincterotomy
- Balloon and basket gallstone extraction
- Mechanical or laser gallstone fragmentation
- Stricture balloon dilatation
- Plastic/Metal biliary stenting
- Nasobiliary drainage
- Cholangioscopy, biopsy
- Endoscopic cystogastrostomy, necrosis debridement
- Endoscopic ampullectomy
- Pancreatic sphincterotomy
- Pancreatic duct balloon dilatation
- Pancreatic stenting
- Pancreatic stone fragmentation, stone extraction
*In our HPB center, ERCP procedures are performed with 99% success and 3% pancreatitis complication.
How is ERCP Performed?
ERCP is an endoscopic procedure that is sometimes necessary for the diagnosis but mostly for the treatment of hepatopancreatobiliary diseases. ERCP procedure is performed with the following steps:
How Should Patient Preparation Be Before ERCP?
Blood tests: Biochemical tests, liver enzymes, cholestasis enzymes and bilirubins, hemogram, PT, INR and APTT should be requested in all patients before ERCP. These tests should not exceed 1 week. Hemogram and INR results should not exceed 3 days in jaundiced patients. INR<1.5 in non-urgent cases, INR between 1.5-2 in urgent cases. ERCP is contraindicated if INR>2. PLT count should be over 100,000 if possible.
Blood thinners: Aspirin and other potent antiplatelets should be stopped 5-7 days in advance. If using coumadin and new oral anticoagulants, they should be stopped and low molecular weight heparin (LMWH) administered by injection should be started instead.
Radiological examinations: Radiological examinations should be complete, ERCP should be performed for therapeutic purposes rather than diagnostic purposes. There should be at least liver, gallbladder, bile ducts and pancreatic USG. USG alone often does not provide sufficient information for ERCP and additionally contrast CT or contrast MR-MRCP should be requested before ERCP. ERCP should not be performed without contrast CT or Contrast MR in patients with a possibility of tumor and if ERCP is recommended, this decision should be made after seeing an HPB surgeon. ERCP is not performed only to correct jaundice in most periampullary tumors!!!!
Fasting: 6-8 hours of fasting is required. In fact, this is not related to the ERCP technique, but is important due to the risk of sedation and aspiration and the discomfort it causes to the patient.
Consent: Informed consent must be obtained from all patients.
If possible, a vascular access should be established on the back of the right hand before the procedure, a triple tap should be placed in between, and fluid infusion should be performed to keep the vascular access open.
Prophylactic antibiotics are generally preferred.
How is Anesthesia Applied in ERCP?
The ERCP procedure is usually performed under either light sedation or deep sedation to ensure comfort. Rarely, if the procedure is difficult and long in elderly and debilitated patients or in infants and young children, it can be performed with general anesthesia by intubation. Noninvasive monitoring should be performed in patients undergoing sedoanalgesia, TA should be checked at 5-minute intervals, and pulse, O2 saturation, and respiratory rate should be monitored continuously. ECG monitoring should be performed during deep sedation. Nasal O2 should be administered continuously to each patient. Conscious sedation can be achieved with midazolam (Dormicum) 2mg plus pethidine (Dolantin) 25-50mg IV, and deep sedation can be achieved with propofol 1-2mg/kg IV. Our preference is deep sedoanalgesia with propofol.
Inserting the Endoscope
To begin the procedure, a thin, flexible, side-viewing tube called a Duodenoscope is used. The endoscope is advanced through the mouth into the mouth, esophagus, and stomach. The endoscope is then directed toward the section called the duodenum. The Papilla Major, which opens into the bile ducts and pancreatic ducts in this area, is found. It is cannulated with special ERCP catheters.
Injection of Contrast Agent
A contrast agent (usually iodine-based) is administered into the cannulated bile ducts and pancreatic ducts under X-ray and scopy. With the contrast agent, the current disease status of the bile ducts or pancreatic ducts is revealed and the necessary treatment decision is made and applied at the same time.
Endoscopic Procedure, Treatment
If an intervention is considered, endoscopic sphincterotomy is often performed first. The following procedures can then be performed:
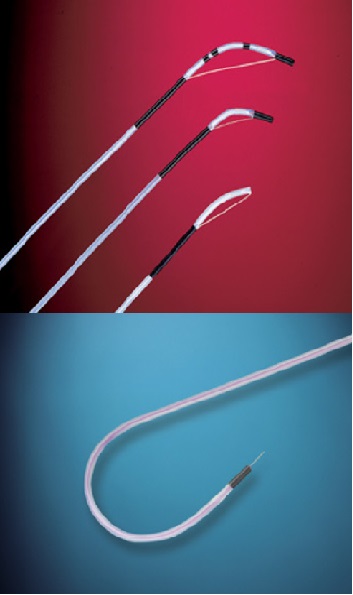
Gallstone Removal: Stones in the bile ducts can be removed with balloons or basket catheters. Large stones can be broken with laser or mechanical means.
Stent Placement: If there is expansion or obstruction in the bile or pancreatic duct, a stent (metal or plastic tube) can be placed to provide flow. This stent keeps the duct open.
Dilatation: A narrowed bile duct or pancreatic duct can often be widened with a balloon or bougie.
Taking a Biopsy: If a tumor is suspected, it is removed via endoscopy.
Other Endoscopic Interventions: Ampouleectomy, cystogastrostomy, etc.
How is Observation and Follow-up After ERCP?
In our country, the vast majority of outpatient cases are followed up as outpatients. The patient who feels comfortable after the procedure under light sedation can be given water orally within 1-2 hours and if tolerated comfortably, can be sent home or back to the hospital where the procedure was sent, depending on the type of procedure. However, after a difficult ERCP or if complications occur, the patient should be hospitalized for at least 1 day, hemogram and amylase should be checked for 1 day, and abdominal pain, fever, and vomiting should be investigated clinically.
Who Can Get ERCP? What Are ERCP Indications?
ERCP is used in the diagnosis and treatment of hepatopancreatobiliary diseases, the situations in which it is performed in terms of diagnosis and treatment are summarized below:
ERCP INDICATIONS (The SAGES Manual,1999 modified
Vater ampulla visualization
Adenoma, carcinoma
Patients with polyposis syndrome
IPMN
Cholangiography
Cholestatic jaundice of unknown cause
Choledocolithiasis
Cholangitis
Bile duct cancer
Bile duct stricture
Bile duct injury
pancreatography
chronic pancreatitis
pancreatic cancer
pancreatic acid
Pancreatic pseudocyst
pancreatic trauma
Biliary pancreatitis
acute pancreatitis
TREATMENT/THERAPEUTIC ERCP (SAGES, Modified)
Endoscopic Sphincterotomy
Choledocholithiasis
Cholangitis
Papillary stenosis
Sphincter of Oddi dysfunction
Before stent or balloon dilatation
Sump syndrome
Choledochocele
Biliary pancreatitis
Stent placement
Benign or malignant stricture
Biliary and pancreatic fistulas
Postoperative bile leak
Large, unremovable choledochal stones
Nasobiliary Drain Application
Pallation of jaundice in Klastkin tumor
Prevention or treatment of acute cholangitis
Postoperative bile leakage (if stent failure)
Definitive treatment of ruptured hydatid cyst in bile ducts
Cholangioscopy, biopsy, laser lithotripsy
Cystogastrostomy, Necrosectomy
Pseudocyst
Walled pancreatic necrosis
Ampullectomy
Ampullar tumor
Balloon dilatation
Bile duct stricture
Ampullar dilatation
Diseases treated with ERCP
Bile duct stones (choledocholithiasis)
One in 10 patients with gallbladder stones also have stones in the common bile duct, and this rate increases to 25% in those over the age of 60. Every patient who will undergo gallbladder surgery should be checked for hidden stones in the bile duct. Untreated bile duct stones can cause fatal complications such as jaundice, cholangitis, liver abscess and acute pancreatitis.
ERCP is currently the gold standard in the treatment of common bile duct stones and is most commonly performed for this purpose. In experienced hands, it can be performed with a duodenoscope in 10-30 minutes with 98-99% success. Endoscopic sphincterotomy is performed with a special catheter to open the mouth of the bile duct, and stones smaller than 1.5 cm are dropped into the duodenum with a balloon and basket catheter. If the stone is larger than 1.5 cm, it is broken with a device called a lithotripter and evacuated in pieces. Most patients can be fed 2-3 hours after ERCP and are discharged the same day.
Cholangitis: Inflammation of the bile duct
Delay in treatment is a disease that can result in death in 1 in 10 patients. It is often due to gallstones. Treatment is provided by ERCP with sphincterotomy stone extraction and, if necessary, biliary stenting-nasobiliary drainage.
Bile duct strictures and Bile fistulas
Bile fistulas and bile duct strictures are most commonly seen due to laparoscopic cholecystectomy. In addition, fistulas may also develop after liver surgeries. Fistulas heal with ERCP and endoscopic sphincterotomy, biliary stenting may be required in the presence of high-output fistulas or bile duct damage.
Obstructive jaundice due to periampullary tumors (pancreas, bile duct and duodenum)
Jaundice is often resolved by applying plastic or metal stents with ERCP.
Collections due to pancreatitis: Pseudocyst and Walled Necrosis (WON)
The treatment we apply in cases of pancreatic pseudocysts and WON is often Transgastric Endoscopic Cystogastrostomy. Treatment is done with plastic in pseudocysts and temporary metal stenting in WON.
Recurrent pancreatitis due to pancreas divisium
Minor papilla sphincterotomy and pancreatic stenting are performed with ERCP
Wirsung stenosis and pancreatic stones due to chronic pancreatitis
ERCP, pancreatic sphincterotomy, stone extraction are performed. If there is stenosis, Wirsung duct is dilated with a balloon and plastic pancreatic stenting is performed.
ERCP in patients with gastric resection
ERCP in patients with Bilroth II gastroenterostomy is quite difficult and the complication rate is high. Our HPB clinic has the most experienced team in such patients, ERCP has been performed on over 100 patients with gastric resection.
ERCP in Infants
For the first time in Turkey, ERCP, Sphincterotomy, stone extraction, biliary balloon dilatation and biliary stenting procedures were performed on an infant by Prof. Dr. Kemal Dolay. ERCP is performed on infants and children with special thin-diameter endoscopes and under general anesthesia.
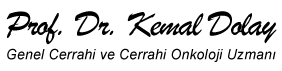
What are the Instruments and Catheters Used During ERCP?
Special Duodenoscopes, ERCP catheters, Guide wires, Balloon and Basket catheters, Stents, Nasobiliary drains and other endoscopy devices are used during ERCP. A special radiology table and C-Arm X-ray scopy device are required.
DUODENOSCOPES
Duodenoscopes have a side view. In addition to the Up-Down Right-Left button, there is an elevator for directing catheters used for cannulation and intervention. The working channel of standard duodenoscopes is 3.2 mm, the outer diameters are 10.8 in the shaft section and 12.5 mm in the manipulated tip section. The working channel of therapeutic duodenoscopes is 4.2 mm or 4.8 mm. The outer diameters are less than 12 mm in the shaft section and 13.1 mm in the manipulated tip section. The working channel of jumbo duodenoscopes is 5.5 mm. The outer diameter of pediatric duodenoscopes is 7.4 mm and the working channel is 2.2 mm in diameter.

ERCP CANNULAS
Primary cannulation of papilla and common bile duct
Standard cannulas
–5F and 7F diameter
–can be straight, curved and rounded tipped
–0.035-inch guide wire can be passed. Contrast can be given from the guide side in 3-lumens.
Tapered or ultra-tapered cannulas
–they allow better cannulation in some cases,
–however, ultra-tapered cannulas only allow passage of 0.025-inch guide.
There is no strong study showing a difference between standard and tapered cannulas in terms of cannulation success. The risk of submucosal injection is slightly higher with tapered tipped catheters.

SPHINCTEROTOMS
Standard sphincterotome: The cutting wire can be a monofilament wire or a braided wire. The difference is that a single wire cuts faster, but can easily break and deform quickly due to the cautery.
Precut sphincterotome.
Needle-knife papillatome
Sphincterotomes with insulated cutting wire: prevents uncontrolled cutting, cautery injury and short circuit
There are also sphincterotomes with ready-made guide wires or balloons
GUIDE WIRES
Guide wires are the most vital materials of the ERCP procedure. They can be used to achieve cannulation, as well as to continue the achieved cannulation during the procedure, to send a sphincterotome, balloon and basket over it, stenting, nasobiliary drainage, biliary dilatation, etc., all procedures are performed over the guide wire.
The wire inside the guide wires is made of nitinol, and the part at the tip is made of platinum. Platinum was used because it looks more opaque under scopy. The outer part is usually teflon-coated to reduce friction and to avoid unwanted situations such as cautery injuries and short circuits during sphincterotomy. The tip can be straight or J-shaped. In addition to those with slippery and flexible tips, there are also nitinol-shaped guide wires that are particularly hard for stent placement and dilatation purposes. Hydrophilic-tipped guide wires are more useful, especially in strictures or malignancy-related stenoses. They can be 0.018, 0.025 and 0.035 inches in diameter and 260-480 cm in length. In a standard ERCP, straight-tipped Zebra guidewires with a diameter of 0.035 inches and a length of 480 cm are generally used.

STONE QUARRYING MATERIALS Balloons and Baskets
Balloon catheter
–5-6.8F catheter, 8-18mm balloon diameter, double lumen
Dormia basket
–4-6 wire, steel mesh or nitinol
–Basket that can sometimes be guided in IHSY stones
Lithotripsy basket
–1.5cm< stones, stone-distal choledochus incompatibility
–Basket and lithotripter separately or as a single set
DRAINAGE MATERIALS: Stent (Plastic, Metal: SEMS), NBD
STENT
–Plastic: Temporary drainage, stenosis, life span 3 months, Diameter: 5, 7, 8.5, 10 and 11.5F, Multiple flap, single flap
–Metal: SEMS Patensi 6-9 months, TTS, catheter 8.5F, 10mm diameter, coated, uncoated
NBD (nasobiliary drainage) Catheter
-5, 7 and 10 F, 5-9 side holes at the tip
-In severe purulent cholangitis requiring irrigation and aspiration, stent-resistant biliary fistulas and ruptured hydatid cysts in the bile ducts

What are the Risks and Complications of ERCP?
Although ERCP is generally a safe procedure, it is the most difficult and complex procedure of GI endoscopy and has some risks.
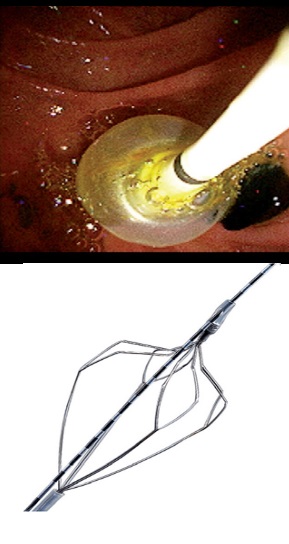
In 1991, the consensus defined and classified ERCP complications as: pancreatitis, bleeding, perforation, infection and basket impaction.
However, in 2010, all associations related to ERCP (ASGE, AGA, SAGES, NCI, NIH, NSQIP etc.) came together and defined them as Adverse Events instead of complications. The aims here are: to cover all events, standardization and medicolegal protection. An event that prevents the completion of ERCP, requires hospitalization, prolongs the hospital stay, requires another procedure (requiring sedation/anesthesia) or additional medical consultation is defined as an Adverse Event.
In ERCP, General Complications are 7-12%, Serious Complications are 2% and Mortality is 01-1.4%, and most deaths occur after 30 days and most are due to the underlying disease (75% cancer).
Pancreatitis: It is the most common complication after ERCP, with an average of 5%. When managed well, it does not often lead to death.
Perforation, Puncture: This is the most serious complication, its frequency is less than 1% but the mortality rate is 10%.
Infection: There is a risk of infection during endoscopy.
Bleeding: There is a risk of bleeding in interventions performed via endoscopy, but it does not usually cause a problem.
Bile Duct Rupture: A small tear may occur in the bile ducts, which can be corrected at the time of the procedure with stenting.
In conclusion, ERCP is a very effective method in the treatment of HPB diseases and generally offers a solution that does not require surgical intervention. However, since it carries a risk of death, it is very important that advanced ERCP procedures are performed by experienced hands and by doctors who are competent in this field.
How Many Hours Does an ERCP Procedure Take?
The ERCP (Endoscopic Retrograde Cholangiopancreatography) procedure is a procedure that usually takes between 5 and 30 minutes, depending on experience and the difficulty of the procedure required. However, the duration of the procedure may vary depending on the complexity of the intervention, the time it will take, and the difficulties in the procedure.
ERCP and Surgical Endoscopy Treatment Process with Prof. Dr. Kemal DOLAY
ERCP (Endoscopic Retrograde Cholangiopancreatography) and Surgical Endoscopy are advanced endoscopic techniques used in the treatment of serious health problems in HPB and other GIS organs. These advances are of great importance in the treatment of conditions such as obstructions, stones, strictures or cancer in the bile ducts, pancreatic digestive tract and other parts of the digestive system. Prof. Dr. Kemal DOLAY is an HPB surgeon and surgical Endoscopist with extensive experience in this field, having performed more than 7000 ERCPs in total. He has also trained many specialists in the field of ERCP. He has organized numerous ERCP courses and meetings in Turkey and internationally. Many of his publications have been cited in international journals and books, and recommendations have been made in international guidelines regarding ERCP, referring to his work.
Prof. Dr. Kemal DOLAY evaluates patients who apply for ERCP in detail, examines both the reports and films of their blood and radiological examinations, consults the radiology professor he works with on this issue if he deems it necessary, and finally puts an indication if ERCP is necessary. He explains the ERCP procedure and possible complications to the patient and relatives in detail. After receiving the patient’s consent, he successfully performs the ERCP procedure. After the ERCP procedure is completed, he shares the results and reports with the patient and relatives and usually discharges the patient after monitoring him in the hospital for a while. His advanced experience in this field results in high success and low complications in the ERCP procedure.
Repeat Checks: Patient checks are recommended after ERCP.
Lifestyle and Diet Adjustments: The patient’s diet and lifestyle are important factors for the success of the treatment process. Healthy nutrition, regular exercise and stress management can be recommended.
Advanced ERCP and Surgical Endoscopy treatment process is personalized according to the type of intervention and complication risks by expanding it. Prof. Dr. Kemal DOLAY ensures a high level of competence for patients at every stage throughout this process. The completion of the treatment process with Advanced ERCP is achieved with correct diagnosis, expert management and follow-up.
Is ERCP Safe in Pregnant Women?
ERCP in Pregnancy
The risk of gallstone formation increases due to hormonal changes, increased cholesterol levels and delayed emptying of the gallbladder during pregnancy. The incidence of gallstones during pregnancy is between 3-12%. Most pregnant patients are asymptomatic and do not require treatment. Rarely, gallstones or sludge in the gallbladder fall into the bile duct, causing biliary colic, biliary pancreatitis, obstructive jaundice and purulent jaundice, namely cholangitis.
Acute cholangitis and pancreatitis due to stones during pregnancy are life-threatening conditions for both the mother and the fetus and often require emergency intervention. Endoscopic retrograde cholangiopancreatography (ERCP) sphincterotomy and stone extraction are the standard approaches in the treatment of bile duct stones. While the ERCP procedure involves procedure-related risks for the mother, it also has the potential to harm the fetus due to exposure to ionizing radiation. It is necessary to take protective measures to protect the fetus from radiation membrane, keep the fluoroscopy time short or apply radiation-free ERCP techniques when possible.
The most common indications for performing therapeutic ERCP during pregnancy are symptomatic choledocholithiasis, obstructive jaundice, biliary pancreatitis, and acute cholangitis.
*When deciding to perform ERCP on a pregnant woman, the indication must be definite.
*The patient must be informed in detail and consent must be obtained.
*A gynecologist consultation and fetal monitoring must be provided before, during and after the procedure.
*With MRCP, the anatomy of the bile ducts, the size and number of common bile duct stones and the distal common bile duct diameter must be revealed and a decision must be made before the procedure on what to do in ERCP.
*When the pregnant woman is placed on the ERCP table, the area below the navel must be surrounded with lead sleeves for protection from possible scopy.
*ERCP must be kept short and the most minimally invasive procedure must be preferred. In difficult stones, direct plastic stenting may be preferred without dealing with breaking them. Difficult procedures are planned after birth.
* In the selection of drugs for sedoanalysis, the safety of the fetus must be taken into consideration and the pain and concerns of the expectant mother must be relieved.
Prof. Dr. Kemal Dolay performed successful and uncomplicated ERCP and stone removal procedures in 6 pregnant patients, and directly placed a plastic stent in one patient because of a difficult stone, requiring a single short scopy once. All patients were discharged without any problems and their births were on time and healthy as planned.
ERCP in Children and Infants
While ERCP in children was rarely performed in the past, in the last twenty years there has been an increase in the incidence of acute and chronic pancreatitis and gallstones and related complications in children. Therefore, ERCP experience in children and infants is increasing. In Tables 1 and 2 you can see a summary of congenital and acquired hepatopancreatobiliary anomalies and diseases and diseases that may require ERCP.
Table 1: Anatomical Abnormalities Associated with Pancreatitis in Children
|
Table 2: Potential ERCP Indications in Children
|
ERCP in children and babies requires a high level of expertise and special training. While ERCP can be performed with the same endoscope and catheters in children, a special thin endoscope is required for ERCP in very weak children or babies. Also, it is safer to perform ERCP under full general anesthesia and intubation in young children and babies than in adults.
Prof. Dr. Kemal Dolay has safely and successfully performed ERCP on more than 15 children. He also made history by performing ERCP on an 11-month-old baby for the first time in Turkey.